Uncategorized
What to look for in Prenatal Vitamins?
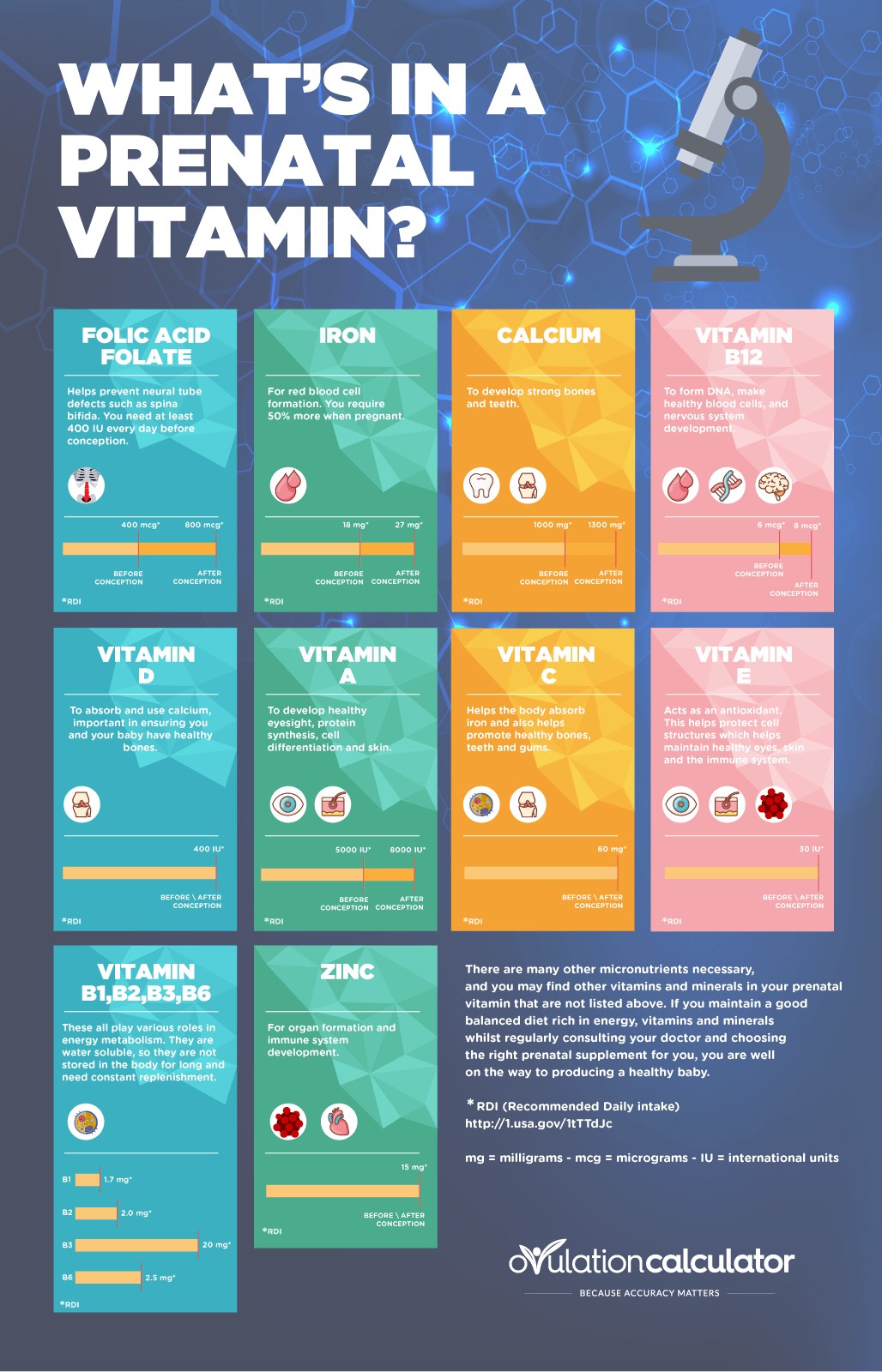 Until recently, the main supplements recommended for pregnancy were folic acid and iron. Increased blood volume and the developing placenta place large demands on iron stores, and maternal folic acid (ideally taken before conception) helps prevent spina bifida and other neural tube defects.
Until recently, the main supplements recommended for pregnancy were folic acid and iron. Increased blood volume and the developing placenta place large demands on iron stores, and maternal folic acid (ideally taken before conception) helps prevent spina bifida and other neural tube defects.
In recent years, the National Institute of Health (NIH) lists recommended daily intakes of various nutrients for pregnant and breastfeeding women based on the latest available scientific evidence. The key nutrients for pregnant women are as follows:
Iron
Pregnancy increases the need for iron in the diet. Apart from increased vascular blood mass for the mother and placenta, the developing fetus draws iron from the mother for use in the first five or six months after birth too. Although studies show that absorption of iron can increase substantially during pregnancy, the recommended daily intake (RDI) is set at 27mg, and vegetarians, vegans and women carrying more than one baby are at risk of iron deficiency.
Folic acid
The RDI for women is 600 micrograms (mcg) for one month before conception and for three months after. Supplement is recommended, as are natural sources such as green vegetables and whole grains. The general recommendation is that in addition to eating folate-rich foods, women planning a pregnancy or in their first trimester should take a daily supplement containing at least 400mcg (preferably 500mcg) of folic acid.
Iodine
Iodine is necessary for the normal growth and mental development of a baby, and the RDI for pregnant women is 220mcg and 270mcg for breastfeeding women. After milk producers switched from using iodine-based to chlorine-based cleaners to clean dairy equipment, and more people ditched iodised table salt for gourmet salt – or none at all – iodine deficiency became an issue, with pregnant woman in parts of the country suffering mild to moderate deficiency in the early 2000s.
Since 2009, bread manufacturers have been required to use iodised salt in all bread except organic bread. However, on its own this won’t ensure pregnant or lactating women are getting enough iodine, and a 150mcg supplement is recommended.
Vitamin D
Vitamin D helps the body absorb and use calcium. The most recent recommendations are that an adequate intake (AI) for all adults up to the age of 70, including pregnant and lactating women, is 15mcg (or 600 international units) of dietary vitamin D per day.
Calcium
A developing fetus needs calcium for healthy bones, teeth, muscles, nerves and their heart. Normal levels of recommended calcium intake will suffice, although pregnant teenagers will need extra. Women who avoid dairy products or have a vitamin D deficiency may need a supplement.
Vitamin B12
Vitamin B12 is needed for neurodevelopment. It’s only found in animal products (meat, eggs and dairy) and some types of algae, so vegans may need vitamin B12 daily supplementation of 250-500mcg.
Omega 3 fatty acids
Many supplements contain fish oil, which provides omega-3 fatty acids essential for the baby’s neural development. Total omega-3 recommended per day is up to 1.4g.
Supplements for morning sickness
Morning sickness affects between 50-80% of women in early pregnancy. Advice for treating it includes eating dry foods, having small, frequent snacks, and avoiding food or situations that cause nausea.
Vitamin B6 and ginger are often recommended to help relieve nausea and vomiting. A large review of studies found that these may help relieve the nausea, but not necessarily the vomiting associated with morning sickness.
Other herbal supplements commonly used by women for morning sickness relief include peppermint, chamomile, and red raspberry leaf, with acupressure and homeopathy, among other alternative therapies used.
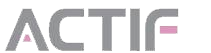
What to eat while pregnant?
Clinical trials have shown the benefit of taking vitamins and mineral supplements designed for pregnancy. The main benefits reported are reduced risk of neural tube defects and maternal anaemia. Where there’s a risk of malnutrition, supplements have been shown to reduce the risk of low-birth-weight babies.
If your diet is generally healthy, with plenty of fruit, vegetables, nuts, pulses and dairy products (or calcium-fortified alternatives), you’re unlikely to benefit from a pregnancy supplement. There are lots of nutritional benefits from food that can’t be obtained from a vitamin pill – and no pill will undo the negatives of a diet of pies, chips and chocolate.
The reality, however, is that many women – pregnant or not – don’t have a diet that’s entirely healthy, and some women struggle to eat well if they suffer severe morning sickness, in which case the extra nutrients in pregnancy supplements may be useful.
Herbal medicines in pregnancy – What to avoid
Herbal medicines are often perceived to be natural and safe, but there’s not much information about the safety and effectiveness of these products in pregnancy, and many women taking them don’t tell their doctor.
There’s very real cause for concern, with numerous studies linking herbal medicines with adverse effects in pregnancy. For example, a large study found that using almond oil to prevent stretch marks was linked with increased risk of premature birth, while liquorice may be linked to threatened miscarriage and premature birth. Common Chinese herbal medicines, especially when taken in early pregnancy, have been linked with growth and developmental abnormalities in baby mice, and some have also been linked with human abnormalities.
The Royal Women’s Hospital in Melbourne recommends avoiding, or exercising caution with, the following herbal medicines:
- Aloe vera is OK as a topical gel, but aloe vera latex taken orally in powder or liquid form may cause low blood sugar, uterine contractions, or miscarriage. There’s not enough information about safe doses in pregnancy, so it’s probably best to avoid aloe vera juice and supplements.
- Black cohosh may cause early labour, so avoid in early pregnancy.
- Evening primrose oil has limited safety information.
- Garlic as used in a cooking is fine, but avoid large doses in supplements, as they may cause bleeding, miscarriage or early labour.
- Ginseng should be avoided during pregnancy, especially early pregnancy, as it can cause serious adverse reactions.
- Liquorice in large quantities, as in liquorice extract or liquorice root, can cause miscarriage and early labour. Black liquorice sold as confectionery may contain the extract, or may be flavoured with aniseed.
- St John’s Wort may reduce your baby’s birth weight, and interferes with certain medicines. Talk to your doctor before taking it while pregnant.
- Valerian has limited safety information about taking it in pregnancy. Talk to your doctor first.
Breastfeeding
After the baby’s arrival, you won’t need extra nutrients such as iron, but you’ll need more of some other nutrients, including vitamins A, all the B complex vitamins, C and E, and especially iodine. A healthy diet and increased appetite should ensure adequate levels of most of these nutrients, although an iodine supplement may be necessary.
What about conception?
There are several micronutrient formulations available for women and men trying to conceive.
For women, a folic acid supplement is recommended for one month prior to conception to reduce risks of neural tube defects. There’s no need for any other special supplement at this stage, although if your diet isn’t as healthy and balanced as it should be, now’s the time to start good habits to see you through pregnancy and family life.
For men, small studies with low numbers of live births suggest that antioxidants create healthier sperm, and men with low fertility have been found to have lower levels of antioxidants in semen than fertile men. Antioxidant supplements containing vitamins and minerals, such as vitamin E, vitamin C, carotenoids, ubiquinol, folate and zinc are commonly used for increasing the chances of conception.
Humans produce their own antioxidants and also get some from plant foods, especially fruit and vegetables. Other contributors to poor sperm health include excessive exercise, alcohol, smoking, drugs, stress and environmental pollution, so this might be the time to spring clean your lifestyle!